Glaucoma Treatment
for Patients in Tyler, Athens, Longview, TX & All of East Texas
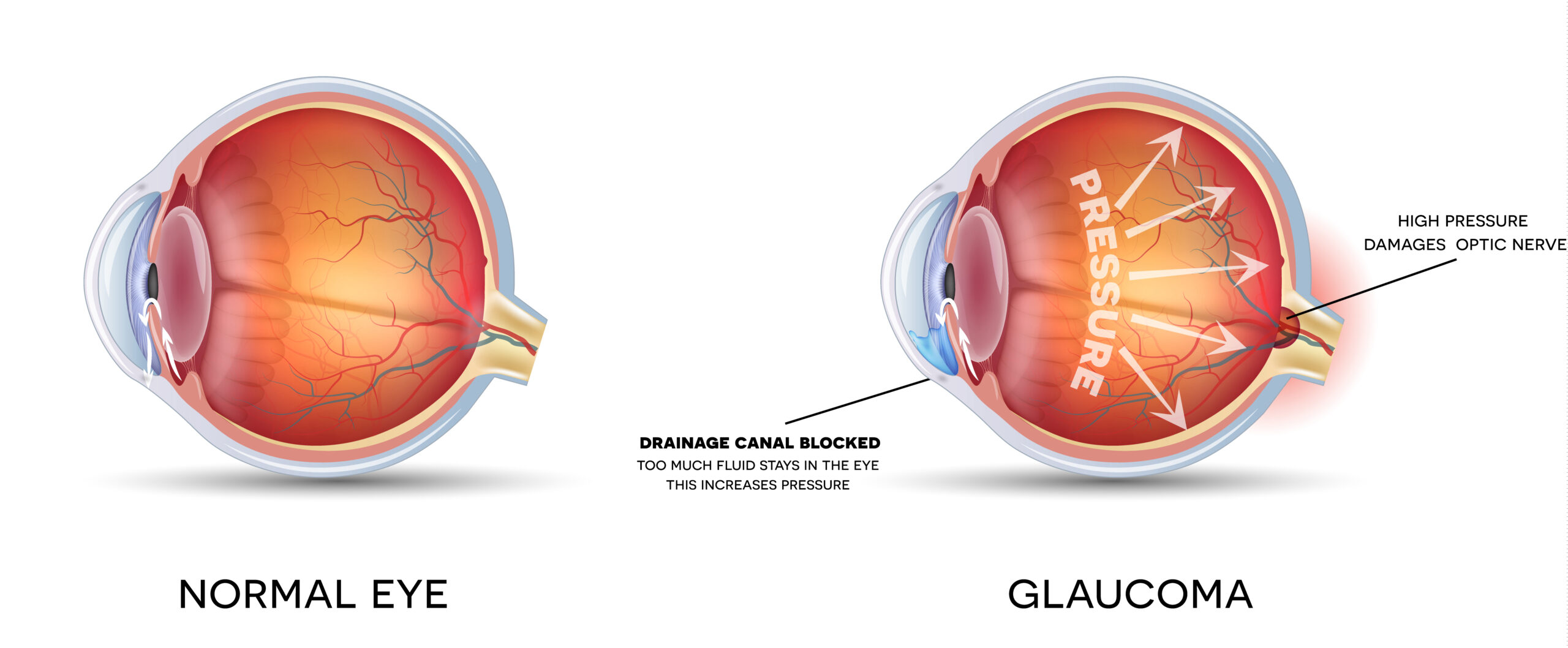
Glaucoma is a disease regarded as optic nerve damage. The optic nerve damage produces peripheral vision loss associated with higher than “normal” intraocular pressure. Glaucoma often referred to as a Silent Thief of Sight, is estimated to impact over 4 million Americans with only half of those people knowing they have the disease.
It is the second leading cause of blindness in the world. However, if caught early, it can be effectively treated. Glaucoma can occur at any age. And, the risk of developing the disease increases dramatically after age 35. One in every 50 adults is estimated being affected by this disease.
Glaucoma is a series of diseases that damage the optic nerve. Damage to the optic nerve and retina causes blind spots in the field of vision. Glaucoma is usually caused by an increase in the fluid pressure in the eye, either because of overproduction of fluid or from a blockage in the drainage system of the eye. The higher pressure inside the eye causes damage to the optic nerve, resulting in permanent vision loss.
Don’t wait for your vision to worsen. If you suspect you have early signs of glaucoma or would like to schedule a comprehensive eye exam, please feel free to contact Heaton Eye Associates! Our team of ophthalmologists have the experience and state-of-the-art technology to help identify, address, and perform glaucoma treatments for patients throughout Tyler, Athens, Longview, Beaumont, Bryan, College Station, Conroe, Dallas, Houston, Jacksonville, TX, and all of East Texas.
The early symptoms of chronic open-angle glaucoma, the most common type of glaucoma, are often unnoticed because there is no discomfort or pain. Most people will not notice a change in vision until there is a significant loss of vision. Later, central vision becomes affected, with mild headaches and difficulty with night vision. If left untreated, total blindness will result. However, the patient with acute closed-angle glaucoma may experience more noticeable symptoms including blurred vision, severe pain, nausea, and halos around lights.
In most cases, our doctors can detect glaucoma in a routine eye examination. Glaucoma is detected using special instruments. One instrument checks the fluid pressure in the eye. Then a magnifying lens is used to examine the drainage channels for proper fluid outflow. Early detection and treatment can almost always control glaucoma and preserve vision. Sadly, there is currently not a cure for glaucoma. Your vision, once lost, is impossible to restore. Remember, glaucoma vision loss is permanent. But, can usually be prevented with early detection and treatment. Regular eye exams are important for people over 35, or those in other high-risk groups.
Risk Factors For Glaucoma
The following are risk factors as outlined by the Mayo Clinic
Elevated Internal Eye Pressure (Intraocular Pressure)
If your intraocular pressure is higher than normal, there is an increased risk for you to develop glaucoma, but not everyone with elevated intraocular pressure develops the disease.
Age
Everyone older than 60 is at increased risk of glaucoma. For certain population groups such as African-Americans, the risk is much higher than expected. African-Americans should begin to have their eye pressure monitored before age 30.
Ethnic Background
African-Americans are six to eight times more likely to get glaucoma than Caucasians and are much more likely to experience permanent blindness as a result. Hispanic-Americans also face an increased risk. Asian-Americans are at slightly higher risk of angle-closure glaucoma, and Japanese-Americans are at a greater risk of developing low-tension glaucoma. The reasons for these differences in elevated risk aren’t clear.
Family History of Glaucoma
You have an increased risk of developing glaucoma if there is a family history. Glaucoma may have a genetic link, meaning there’s a defect in one or more genes, causing certain individuals to be unusually susceptible to the disease. There is a clear link between juvenile open-angle glaucoma and genetic abnormalities.
Medical Conditions
Diabetes increases your risk of developing glaucoma. A history of high blood pressure or heart disease also can increase your risk, as can hypothyroidism.
Other Eye Conditions
You have an increased risk of developing glaucoma if there is a family history. Glaucoma may have a genetic link, meaning there’s a defect in one or more genes, causing certain individuals to be unusually susceptible to the disease. There is a clear link between juvenile open-angle glaucoma and genetic abnormalities.
Nearsightedness
Nearsightedness (meaning objects in the distance look fuzzy without glasses or contacts) increases the risk of developing glaucoma.
Prolonged Corticosteroid Use
Using corticosteroids for prolonged periods of time appears to put you at risk of getting secondary glaucoma. Getting secondary glaucoma is especially true if using corticosteroid eye drops.
Glaucoma Treatment Options
Laser Treatment Options
SLT (Selective Laser Trabeculoplasty)
Selective Laser Trabeculoplasty (SLT) is a safe and effective way to treat glaucoma. The laser works by opening up channels in the trabecular meshwork and utilizing the natural drainage system in the eye. It is an easy procedure done in our office and only takes minutes to do. Recovery time is typically rapid, with little to no discomfort.

MicroPulse® Laser Trabeculoplasty
With MicroPulse® laser therapy, a continuous-wave laser beam is broken down into a train of short, repetitive, low energy pulses separated by a brief resting period allowing the tissue to cool between laser pulses. This tissue-sparing laser therapy is used to reduce ocular pressure.

Surgical Treatment Options
Trabeculectomy
This classic glaucoma surgical procedure has been performed for many years. This procedure is often recommended when reasonable efforts with medicine and laser have not been effective.
The treatment is performed in our surgery center and takes about an hour. Trabeculectomy involves creating a small channel that allows the flow of fluid to “bypass” the trabecular network and lower intraocular pressure. Recovery time generally takes anywhere from 1 – 6 weeks.
Glaucoma Tube Shunts
With this procedure, a small silicone tube is placed in the eye where fluid is drained to a “plate”where the fluid collects and then is re-absorbed into the body. This technology continues to improve and is an excellent procedure that can help control intraocular pressure and slow the progression of glaucoma.
iStent® with Cataract Surgery
iStent® is the smallest medical device ever approved by the FDA. This tiny implant is placed in your eye during cataract surgery, and is so small, you will not be able to see or feel it after the procedure is complete. iStent® works by creating a permanent opening in your trabecular meshwork, and works continuously to improve the outflow of fluid from your eyes to help control eye pressure.
ABiC™
ABiC™ (ab interno canaloplasty) is a new minimally invasive glaucoma surgery (MIGS). ABiC™ is unique in that it acts to restore the eye’s natural drainage system. ABiC™ addresses several aspects of outflow resistance including Schlemm’s canal and the Collector Channel System. The procedure utilizes a small cathater, iTrack, that is used to canulate the existing drainage pathway. Further information can be obtained at www.glaucoma-itrack.com/treatment-options.
Kahook Dual Blade® (KBD)
The Kahook Dual Blade® is a high-tech, single-use instrument that is used to treat glaucoma, typically performed at the time of cataract surgery. This outpatient procedure is quick and painless, with quicker recovery than most other glaucoma treatments. This technology allows our surgeons to treat glaucoma by making precise, targeted incisions in the eye’s trabecular meshwork tissue for quick and effective glaucoma treatment.
Gonioscopy Assisted Transluminal Trabeculectomy (GATT) with OMNI Device
GATT is a minimally invasive surgical treatment for the management of open angle glaucoma in both adults and children. Dr. Dossey incorporates the OMNI device to carry out this two-part procedure. The first part, visco-canaloplasty, is a procedure that dilates the entire 360 degrees of Schlemm’s canal, allowing drainage channels to function better. The second part, trabeculectomy, removes a portion of the trabecular meshwork, providing direct access for fluid to drain into Schlemm’s canal. Patients at any stage of glaucoma are candidates for this procedure.
Prevention is the Best Medicine
Vision loss from glaucoma is permanent but can usually be prevented with early detection and treatment. Glaucoma management can be a life-long process requiring frequent monitoring and constant treatment. Since there is no way to determine if glaucoma is under control based on how a person feels or their vision, they should be examined every 3 to 6 months.
Medications are extremely safe and effective at treating glaucoma. Medications have multiple mechanisms of action, including slowing down the production of fluids, (turning down the faucet to a sink) or facilitating drainage of fluid from the eye (opening up the drain). The most popular and effective glaucoma medication classes include:

Prostaglandin Analogues
Examples: Xalatan®, Lumigan®, Travatan Z®
These medications work by opening up outflow channels in the eye. They are extremely effective and are only taken one time a day (usually at night). All of these medications can cause red eye, make eye-lashes grow and rarely cause mild pigmentation around the eye.
Beta-Blockers
Examples: Timolol®, Betimol®, Istalol®, Betagan®
These medications have been known to be effective in treating glaucoma for many years. They work by slowing down the production of fluid inside the eye. They are not used in asthmatics or other patients with reactive airway disease. They rarely exacerbate depression.
Carbonic Anhydrase Inhibitors (CAI)
Examples: Azopt®, Trusopt®
These medications work by slowing down the production of fluid inside the eye and bringing down the intraocular pressure. These medications work very effectively when combined with a prostaglandin analogue or a beta-blocker. They rarely have systemic side effects but can cause eye irritation on occasion.
These medications work by slowing down the production of fluid and increasing the outflow of fluid from the eye. These medications can occasionally cause an allergic conjunctivitis with a red eye.
Combination Medications
Examples: Cosopt® (combination of CAI and beta-blocker), Combigan® (combination of alpha agonist and beta-blocker)
These are effective and convenient medications that combine two separate medications in one bottle.




